Currently Empty: $0.00
Abstract
BACKGROUND
Despite advances in defibrillation technology, shock-refractory ventricular fibrillation remains common during out-of-hospital cardiac arrest. Double sequential external defibrillation (DSED; rapid sequential shocks from two defibrillators) and vector-change (VC) defibrillation (switching defibrillation pads to an anterior–posterior position) have been proposed as defibrillation strategies to improve outcomes in patients with refractory ventricular fibrillation.
METHODS
We conducted a cluster-randomized trial with crossover among six Canadian paramedic services to evaluate DSED and VC defibrillation as compared with standard defibrillation in adult patients with refractory ventricular fibrillation during out-of-hospital cardiac arrest. Patients were treated with one of these three techniques according to the strategy that was randomly assigned to the paramedic service. The primary outcome was survival to hospital discharge. Secondary outcomes included termination of ventricular fibrillation, return of spontaneous circulation, and a good neurologic outcome, defined as a modified Rankin scale score of 2 or lower (indicating no symptoms to slight disability) at hospital discharge.
RESULTS
A total of 405 patients were enrolled before the data and safety monitoring board stopped the trial because of the coronavirus disease 2019 pandemic. A total of 136 patients (33.6%) were assigned to receive standard defibrillation, 144 (35.6%) to receive VC defibrillation, and 125 (30.9%) to receive DSED. Survival to hospital discharge was more common in the DSED group than in the standard group (30.4% vs. 13.3%; relative risk, 2.21; 95% confidence interval [CI], 1.33 to 3.67) and more common in the VC group than in the standard group (21.7% vs. 13.3%; relative risk, 1.71; 95% CI, 1.01 to 2.88). DSED but not VC defibrillation was associated with a higher percentage of patients having a good neurologic outcome than standard defibrillation (relative risk, 2.21 [95% CI, 1.26 to 3.88] and 1.48 [95% CI, 0.81 to 2.71], respectively).
CONCLUSIONS
Among patients with refractory ventricular fibrillation, survival to hospital discharge occurred more frequently among those who received DSED or VC defibrillation than among those who received standard defibrillation. (Funded by the Heart and Stroke Foundation of Canada; DOSE VF ClinicalTrials.gov number, NCT04080986. opens in new tab.)
Out-of-hospital cardiac arrest accounts for more than 350,000 unexpected deaths each year in North America; nearly 100,000 of these cardiac arrests are attributed to ventricular fibrillation or pulseless ventricular tachycardia.1 Patients presenting with ventricular fibrillation or pulseless ventricular tachycardia have a higher survival rate than patients with other rhythms. However, despite advances in defibrillator technology, almost half these patients may remain in refractory ventricular fibrillation despite multiple defibrillation attempts.2-5 In these patients, further defibrillation without modification of the defibrillation method is usually unsuccessful. Although antiarrhythmic medications such as amiodarone and lidocaine have been used to prevent refibrillation, neither drug has been definitively shown to improve survival to hospital discharge or neurologically intact survival.6
Double sequential external defibrillation (DSED), the technique of providing rapid sequential shocks from two defibrillators with defibrillation pads placed in two different planes (anterior–lateral and anterior–posterior), has been studied for decades in the electrophysiology laboratory for use in patients with refractory atrial or ventricular fibrillation.7-10 Vector-change (VC) defibrillation, the technique of switching defibrillation pads from the anterior–lateral to the anterior–posterior position, offers the theoretical potential to defibrillate a portion of the ventricle that may not be completely defibrillated by pads in the standard anterior–lateral position. The use of DSED and VC defibrillation in settings outside the hospital has been described in case reports, observational studies, and systematic reviews.11-16 These reports describe cases or series in which DSED was used as a last-resort therapeutic option for patients who remained in refractory ventricular fibrillation, and therefore these studies may have been confounded by resuscitation time bias or the late application of a defibrillation strategy in a subgroup of patients for whom a positive outcome was unlikely.17 It has been suggested that early application of DSED may be associated with higher rates of termination of ventricular fibrillation and return of spontaneous circulation than standard defibrillation.13 The objective of this trial (Double Sequential External Defibrillation for Refractory Ventricular Fibrillation [DOSE VF]) was to evaluate DSED and VC defibrillation as compared with standard defibrillation in patients who remain in refractory ventricular fibrillation during out-of-hospital cardiac arrest.
Methods
TRIAL DESIGN
We conducted a three-group, cluster-randomized, controlled trial with crossover in six paramedic services (which include approximately 4000 paramedics in total) in Ontario, Canada (Region of Peel, Region of Halton, Toronto, County of Simcoe, Middlesex–London, and Ottawa), from March 2018 through May 2022. These paramedic services provide care to a mix of urban and rural communities with a combined population of 6.6 million and treat approximately 4100 patients with out-of-hospital cardiac arrest annually, of whom 15% present in ventricular fibrillation.18 Prehospital medical care is provided by advanced care paramedics (with standard advanced cardiac life-support skills) and primary care paramedics (with basic life-support skills, including the ability to perform manual defibrillation). In addition to the patients enrolled in the current trial (September 10, 2019, to May 18, 2022), 152 patients who had been enrolled in a randomized, controlled pilot trial (March 8, 2018, to September 9, 2019)19 are included in this analysis. Enrollment was paused on April 4, 2020, and resumed on September 8, 2020, to allow the paramedic services time to address concerns about paramedic safety in performing aerosol-generating procedures during the coronavirus disease 2019 (Covid-19) pandemic. The data and safety monitoring board recommended that the trial be stopped early, on May 18, 2022, because of concerns that longer response times caused by paramedic staffing shortages were interfering with the timely application of the assigned type of defibrillation.
PATIENT RECRUITMENT AND RANDOMIZATION
The trial protocol has been described previously20 and is available (along with the statistical analysis plan) with the full text of this article at NEJM.org. The protocol was approved by the research ethics boards of Sunnybrook Health Sciences Centre, Western University, and the Ottawa Health Science Network; participants were not required to provide informed consent.
All patients who were at least 18 years of age and had an out-of-hospital cardiac arrest and refractory ventricular fibrillation of presumed cardiac causes were eligible for the trial. Refractory ventricular fibrillation was defined as an initial presenting rhythm of ventricular fibrillation or pulseless ventricular tachycardia that was still present after three consecutive rhythm analyses and standard defibrillations separated by 2-minute intervals of cardiopulmonary resuscitation (CPR). Patients with a traumatic cardiac arrest, patients with do-not-resuscitate medical directives, and patients with cardiac arrest due to drowning, hypothermia, hanging, or suspected drug overdose were excluded (Table S1 in the Supplementary Appendix, available at NEJM.org). Randomization was performed at the level of the paramedic service. Random treatment sequences were computer-generated by the coordinating center before the start of the trial. Each cluster (paramedic service) crossed over every 6 months to one of the three treatment groups (standard defibrillation, VC defibrillation, or DSED). During the trial, each service had to cross over to each of the treatment groups at least once (Table S2).
TRIAL PROTOCOL AND INTERVENTION
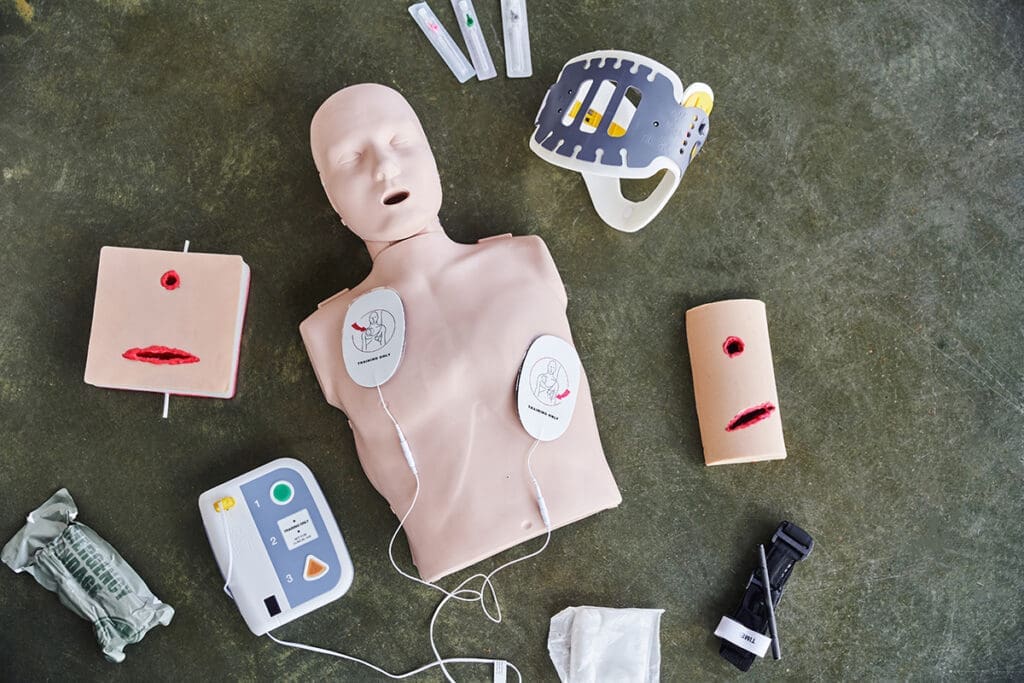
All paramedics followed a provincial protocol consistent with American Heart Association guidelines for the treatment of patients in ventricular fibrillation.21,22 Continuous chest compressions were performed before application of the defibrillator pads. Each rhythm analysis occurred at standard 2-minute intervals. Ventricular fibrillation was determined by manual defibrillator rhythm analysis performed by the paramedics, after which defibrillation was provided. For all patients, the first three defibrillation attempts occurred with defibrillation pads placed in the anterior–lateral position (standard defibrillation). Eligible patients who remained in ventricular fibrillation after three consecutive shocks had been delivered by paramedics or participating fire services (defibrillation shocks provided by fire services were not counted in the pilot trial) received one of three types of defibrillation according to the random assignment for the cluster: standard defibrillation, in which all subsequent defibrillation attempts occurred with the defibrillation pads continuing in the original standard anterior–lateral configuration; VC defibrillation, in which all subsequent defibrillation attempts were delivered with defibrillation pads in an anterior–posterior configuration; or DSED, in which paramedics applied a second set of defibrillation pads (provided by a second defibrillator) in the anterior–posterior position (Figure 1) and all subsequent defibrillation attempts were performed with the use of two near-simultaneous defibrillation shocks provided by two defibrillators. For DSED, to avoid possible defibrillator damage caused by shocks applied at the same instant, a short delay (<1 second) between shocks was created by having a single paramedic depress the “shock button” on each defibrillator in rapid sequence (anterior–lateral followed by anterior–posterior).23
The defibrillation pads were placed in the required configuration as soon as possible during the 2-minute cycle of CPR after the third defibrillation attempt, with minimal interruptions in CPR. The configuration of pad placement and defibrillation is shown in Videos 1 and 2.
TRIAL OUTCOMES
The primary outcome was survival to hospital discharge. Secondary outcomes included termination of ventricular fibrillation, defined as the absence of ventricular fibrillation on subsequent rhythm analysis after defibrillation and a 2-minute interval of CPR; return of spontaneous circulation, defined as any change in rhythm to an organized rhythm with a corresponding palpable pulse or blood pressure documented by paramedics; and a good neurologic outcome at hospital discharge, defined as modified Rankin scale score of 2 or lower (scores range from 0 [no symptoms] to 6 [death]) (Table S3).
STATISTICAL ANALYSIS
We estimated 30-day survival of 28.7% among patients with out-of-hospital cardiac arrest receiving 1 to 3 shocks, declining to 12.4% among those receiving 4 to 10 shocks and 4.9% among those receiving more than 10 shocks.5 We assumed baseline survival of 12% and hypothesized that survival to hospital discharge in the DSED and VC groups would be a minimum of 8 percentage points higher than that in the standard group. On the basis of a fixed number of paramedic service clusters (six), we expected to enroll between 20 and 70 patients per cluster over the course of 1 year. We assumed an intracluster correlation of 0.010 and an interperiod correlation of 0.008 to 0.010 without correction for multiplicity.24-26 Under these conditions, we estimated that 310 patients per group (total sample, 930 patients) would provide 80% power at an alpha level of 0.05.
In this trial, both intervention strategies (DSED and VC defibrillation) shared a common control for comparison (standard defibrillation). The trial design assumed at least two crossovers to allow the three treatment approaches to be tested in each paramedic service. This approach was chosen to maximize efficiency, allowing the evaluation of two new treatments in comparison with usual care in a single three-group, randomized, controlled trial. The primary hypothesis was that each of these strategies would be better than usual care at a P value of less than 0.05 and without correction for multiplicity, as has been recommended for exploratory trials involving multiple treatment groups.25,26 No interim analyses of the primary outcome were performed. All the patients were included in analyses according to their randomly assigned treatment group (intention-to-treat analysis). Prespecified sensitivity analyses included an analysis according to treatment received (regardless of the randomly assigned defibrillation strategy), a per-protocol analysis (involving patients who received the randomly assigned defibrillation at any time after the third shock), and a per-protocol analysis involving patients who were treated with optimal intervention shock timing (defined as three standard shocks followed by the assigned defibrillation strategy as the fourth shock).
Outcomes are reported as adjusted relative risks with 95% confidence intervals, with standard defibrillation as the reference group.27 For analyses of all primary and secondary outcomes, we used generalized linear models with log link and binomial distribution, with a fixed effect for paramedic service and time since starting the trial for each paramedic service used to account for clustering of patients within a paramedic service; all analyses were adjusted for age, sex, and whether bystander CPR was received.28 If this model would not converge for an analysis, we then used modified Poisson regression (see the Supplementary Methods section in the Supplementary Appendix).29-31 An overall test for differences in survival to hospital discharge according to randomized treatment assignment was also performed with the randomization variable in the generalized linear model.
The widths of confidence intervals have not been adjusted for multiplicity, and therefore the intervals should not be used to infer definitive treatment effects for secondary outcomes. No imputation was performed for missing data. A fragility index was calculated with the use of standard equations.32 All statistical analyses were performed with SAS software, version 9.4 (SAS Institute).
PATIENTS
We had enrolled 405 patients before the data and safety monitoring board suggested stopping the trial: 136 (33.6%) were assigned to the standard group, 144 (35.6%) to the VC group, and 125 (30.9%) to the DSED group (Figure 2). Most patients (355; 87.7%) received the type of defibrillation that had been randomly assigned. The mean age of patients in the trial was 63.6 years, and 84.4% were men. A description of the representativeness of the patients included in the trial is provided in Table S4. Overall, 67.9% of out-of-hospital cardiac arrests were witnessed by bystanders and 58.0% of the patients received bystander CPR (Table 1). Resuscitation characteristics (Table S5) and treatment provided are shown in Table 2. The time to first defibrillation and the characteristics of resuscitation were similar in the three groups. Paramedics practiced high-quality CPR during the trial, consistent with current guideline recommendations.33,34 The time and number of shocks to first return of spontaneous circulation were similar in the three groups.
OUTCOMES
A total of 38 patients (30.4%) in the DSED group survived to hospital discharge, as compared with 18 patients (13.3%) in the standard group (relative risk, 2.21; 95% confidence interval [CI], 1.33 to 3.67); the corresponding number in the VC group was 31 patients (21.7%) (relative risk [vs. standard], 1.71; 95% CI, 1.01 to 2.88) (Table 3). In the generalized linear model, the overall test for differences in survival to hospital discharge according to the randomized treatment assignment was significant (P=0.009 for the comparison among the three groups). The results for the termination of ventricular fibrillation, return of spontaneous circulation, survival to hospital discharge, and a modified Rankin scale score of 2 or lower are shown in Table 3. Termination of ventricular fibrillation occurred in 105 patients (84.0%) in the DSED group, as compared with 92 patients (67.6%) in the standard group (relative risk, 1.25; 95% CI, 1.09 to 1.44), and return of spontaneous circulation occurred in 58 patients (46.4%) in the DSED group, as compared with 36 (26.5%) in the standard group (relative risk, 1.72; 95% CI, 1.22 to 2.42). Survival with a good neurologic outcome occurred in 34 patients (27.4%) who received DSED and in 15 patients (11.2%) who received standard defibrillation (relative risk, 2.21; 95% CI, 1.26 to 3.88).
Among the patients who received VC defibrillation, termination of ventricular fibrillation occurred in 115 (79.9%; relative risk [vs. standard], 1.18; 95% CI, 1.03 to 1.36). The return of spontaneous circulation occurred in 51 patients in the VC group (35.4%; relative risk [vs. standard], 1.39; 95% CI, 0.97 to 1.99), and survival with a good neurologic outcome occurred in 23 (16.2%; relative risk [vs. standard], 1.48; 95% CI, 0.81 to 2.71).
The calculated fragility index for the primary outcome suggested that if nine patients in the DSED group or one patient in the VC group had not survived to hospital discharge, the results for the primary outcome would have been rendered nonsignificant. Results of the primary analysis and multiple sensitivity analyses, percentages of patients with a protocol deviation according to paramedic service, and information regarding characteristics of the receiving hospital are shown in Tables S6 through S12. The effect estimates for the primary outcome were consistent across multiple sensitivity analyses.
Discussion
In this randomized, controlled trial of DSED or VC defibrillation for the treatment of refractory ventricular fibrillation during out-of-hospital cardiac arrest, survival to hospital discharge was more common among patients who received DSED or VC defibrillation than among those who received standard defibrillation. Termination of ventricular fibrillation, return of spontaneous circulation, and a good neurologic outcome at hospital discharge appeared to be more common with the DSED strategy, as did termination of ventricular fibrillation with the VC defibrillation strategy. All three groups appeared to be well matched in terms of the timing of drug administration and the mean doses of epinephrine and antiarrhythmic drugs administered, which makes an alternative therapeutic explanation for the trial findings unlikely. Although the outcomes favored DSED, the logistics of having a second defibrillator available may be a challenge in some paramedic services. Given that survival appeared higher with VC defibrillation than with standard defibrillation, the use of VC defibrillation with single-defibrillator systems may be an alternative therapeutic strategy for refractory ventricular fibrillation during out-of-hospital cardiac arrest when a second defibrillator is not available.
Our findings contrast with those of previously reported observational studies and systematic reviews that have shown no benefit of DSED or VC defibrillation as compared with standard defibrillation for patients who have had an out-of-hospital cardiac arrest.15,35,36 However, these studies lacked a control group with standard care characterized by high-quality CPR, did not control for the timing of interventional shocks, did not describe a consistent technique for performing DSED or VC defibrillation, and did not measure or report the quality of CPR performed during DSED or VC defibrillation.
Our trial was implemented in urban and rural areas with 4000 paramedics trained in basic and advanced life support with the use of different defibrillators (manufactured by Zoll Medical or the Stryker Corporation), which suggests that the findings may be broadly generalizable. There was not a single reported case of defibrillator damage or malfunction when DSED was performed. Our trial design involved a common control group for the evaluation of DSED and VC defibrillation for refractory ventricular fibrillation and was meant to provide insight into whether increasing total energy or changing the defibrillation vector would offer greater benefit than standard defibrillation.7-9,37 Our results suggest that although changing the vector of defibrillation (which changes the distribution of voltage gradients during the shock) may have a role in terminating ventricular fibrillation when previous standard defibrillation has been unsuccessful, it is possible that increasing defibrillation energy with the use of DSED also plays a role. Ideker et al. showed that when defibrillation fails to terminate ventricular fibrillation, fibrillation resumes in the region of lowest voltage and current gradient in the myocardium.38 The anatomical location of the left ventricle, a posterior structure, is the region of the heart that is farthest from the direct line between the standard anterolateral electrode pads. VC defibrillation may result in a higher voltage gradient in the posterior part of the left ventricle, where fibrillation is most likely to restart or fail to terminate after defibrillation with standard anterior–lateral pad positions. With DSED, there is the additional influence of increased energy delivered by the second shock. Immediately after unsuccessful defibrillation of the first shock, the instantaneous wave fronts are not the same as they were during ventricular fibrillation and may be more vulnerable to successful defibrillation during the second shock than they would have been if the first “conditioning shock” had not occurred.
Our trial had several strengths, including the cluster-randomized trial design with crossover, which decreased the potential for treatment contamination among the intervention groups, as well as the near-complete outcome ascertainment, continuous performance of high-quality CPR, and the inclusion of outcomes important to patients, including survival to hospital discharge and good neurologic outcome at hospital discharge. In addition, although the treating paramedics had to be aware of the assigned defibrillation strategy, those assessing survival and neurologic outcomes were not aware of the treatment assignments.
This trial also has limitations. The Covid-19 pandemic provided substantial challenges to the paramedics in enrolling patients while donning full personal protective equipment and in some instances performing aerosol-generating medical procedures. The trial did not achieve the planned sample size, since it was stopped early by the data and safety monitoring board as a result of Covid-19–related operational challenges. It is possible that the treatment effect was overestimated, given the small number of events for the primary outcome.39 The trial protocol did not specify a fixed follow-up time, and outcomes were assessed until hospital discharge. The length-of-stay distributions across the trial centers is not known. The benefit of VC defibrillation as compared with standard defibrillation should be interpreted with caution, given the fragility index of 1 for the primary outcome and a less consistent effect with regard to our secondary outcomes and sensitivity analyses. The percentage of patients who received the randomly assigned defibrillation remained consistently high (approximately 90%) throughout the trial. The inability to achieve perfect adherence to the protocol reflects the reality in which paramedics practice. The majority of patients were enrolled in an urban setting, where a second defibrillator is more often available, so the findings may not be generalizable to more remote settings. This trial was completed in the prehospital environment, and information regarding patient race and ethnic group, coexisting conditions, outpatient medication use, or in-hospital treatments was not available. Therefore, it is plausible that there could have been confounding factors that influenced patient outcomes. Finally, the trial was conducted with a high degree of medical oversight and paramedic feedback, which may not be possible in all paramedic services.
Survival to hospital discharge appeared to be higher with DSED and VC defibrillation than with standard defibrillation among patients with refractory ventricular fibrillation during out-of-hospital cardiac arrest.
Author Affiliations
From the Division of Emergency Medicine, Department of Family and Community Medicine (S.C., I.R.D., S.L.M.), the Division of Emergency Medicine, Department of Medicine, (P.R.V., L.J.M.), the Interdepartmental Division of Critical Care Medicine (R.P., D.C.S.), and the Department of Medicine (R.P., P.D., D.C.S.), Temerty Faculty of Medicine, University of Toronto, the Sunnybrook Centre for Prehospital Medicine (S.C., P.R.V., L.T., M.F.), the Departments of Emergency Services (I.R.D., L.J.M.) and Critical Care Medicine (R.P., D.C.S.), Sunnybrook Health Sciences Centre, the Schwartz/Reisman Emergency Medicine Institute, Sinai Health (S.L.M.), and the Division of Cardiology, Unity Health Toronto (P.D.), Toronto, the Division of Emergency Medicine, London Health Sciences Centre, Department of Medicine, University of Western Ontario, London (M.D.), and the Department of Emergency Medicine, Ottawa Hospital Research Institute, Ottawa (C.V.) — all in Canada.
Dr. Cheskes can be contacted at sheldon.cheskes@sunnybrook.ca or at the Division of Emergency Medicine, Department of Family and Community Medicine, Temerty Faculty of Medicine, University of Toronto, 77 Browns Line, Ste. 100, Toronto, Ontario M8W 3S2, Canada.
Reference: https://www.nejm.org/doi/full/10.1056/NEJMoa2207304?query=featured_home